Source(google.com.pk)
Renal And Kidney Biography
The principal function of the urinary system is to maintain the volume and composition of body fluids within normal limits. One aspect of this function is to rid the body of waste products that accumulate as a result of cellular metabolism. Other aspects of its function include regulating the concentrations of various electrolytes in the body fluids and maintaining normal pH of the blood.
In addition to maintaining fluid homeostasis in the body, the urinary system controls red blood cell production by secreting the hormone erythropoietin. The urinary system also plays a role in maintaining normal blood pressure by secreting the enzyme renin.
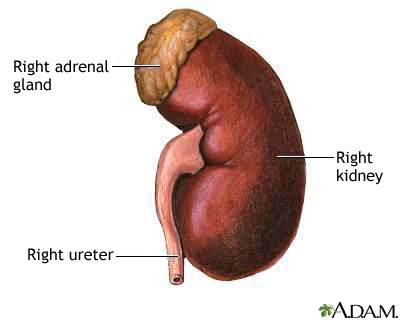
The urinary system consists of the kidneys, ureters, urinary bladder, and urethra. The kidneys form the urine and account for the other functions attributed to the urinary system. The ureters carry the urine away from kidneys to the urinary bladder, which is a temporary reservoir for the urine. The urethra is a tubular structure that carries the urine from the urinary bladder to the outside.
Kidneys
The kidneys are the primary organs of the urinary system. The kidneys are the organs that filter the blood, remove the wastes, and excrete the wastes in the urine. They are the organs that perform the functions of the urinary system. The other components are accessory structures to eliminate the urine from the body.
The paired kidneys are located between the twelfth thoracic and third lumbar vertebrae, one on each side of the vertebral column. The right kidney usually is slightly lower than the left because the liver displaces it downward. The kidneys protected by the lower ribs, lie in shallow depressions against the posterior abdominal wall and behind the parietal peritoneum. This means they are retroperitoneal. Each kidney is held in place by connective tissue, called renal fascia, and is surrounded by a thick layer of adipose tissue, called perirenal fat, which helps to protect it. A tough, fibrous, connective tissue renal capsule closely envelopes each kidney and provides support for the soft tissue that is inside.
In the adult, each kidney is approximately 3 cm thick, 6 cm wide, and 12 cm long. It is roughly bean-shaped with an indentation, called the hilum, on the medial side. The hilum leads to a large cavity, called the renal sinus, within the kidney. The ureter and renal vein leave the kidney, and the renal artery enters the kidney at the hilum.
The outer, reddish region, next to the capsule, is the renal cortex. This surrounds a darker reddish-brown region called the renal medulla. The renal medulla consists of a series of renal pyramids, which appear striated because they contain straight tubular structures and blood vessels. The wide bases of the pyramids are adjacent to the cortex and the pointed ends, called renal papillae, are directed toward the center of the kidney. Portions of the renal cortex extend into the spaces between adjacent pyramids to form renal columns. The cortex and medulla make up the parenchyma, or functional tissue, of the kidney.
The central region of the kidney contains the renal pelvis, which is located in the renal sinus and is continuous with the ureter. The renal pelvis is a large cavity that collects the urine as it is produced. The periphery of the renal pelvis is interrupted by cuplike projections called calyces. A minor calyx surrounds the renal papillae of each pyramid and collects urine from that pyramid. Several minor calyces converge to form a major calyx. From the major calyces the urine flows into the renal pelvis and from there into the ureter.
Each kidney contains over a million functional units, called nephrons, in the parenchyma (cortex and medulla). A nephron has two parts: a renal corpuscle and a renal tubule. The renal corpuscle consists of a cluster of capillaries, called the glomerulus, surrounded by a double-layered epithelial cup, called the glomerular capsule. An afferent arteriole leads into the renal corpuscle and an efferent arteriole leaves the renal corpuscle. Urine passes from the nephrons into collecting ducts then into the minor calyces.
The juxtaglomerular apparatus, which monitors blood pressure and secretes renin, is formed from modified cells in the afferent arteriole and the ascending limb of the nephron loop.
Ureter
Each ureter is a small tube, about 25 cm long, that carries urine from the renal pelvis to the urinary bladder. It descends from the renal pelvis, along the posterior abdominal wall, behind the parietal peritoneum, and enters the urinary bladder on the posterior inferior surface.
The wall of the ureter consists of three layers. The outer layer, the fibrous coat, is a supporting layer of fibrous connective tissue. The middle layer, the muscular coat, consists of inner circular and outer longitudinal smooth muscle. The main function of this layer is peristalsis to propel the urine. The inner layer, the mucosa, is transitional epithelium that is continuous with the lining of the renal pelvis and the urinary bladder. This layer secretes mucus which coats and protects the surface of the cells.
Urinary Bladder
The urinary bladder is a temporary storage reservoir for urine. It is located in the pelvic cavity, posterior to the symphysis pubis, and below the parietal peritoneum. The size and shape of the urinary bladder varies with the amount of urine it contains and with pressure it receives from surrounding organs.
The inner lining of the urinary bladder is a mucous membrane of transitional epithelium that is continuous with that in the ureters. When the bladder is empty, the mucosa has numerous folds called rugae. The rugae and transitional epithelium allow the bladder to expand as it fills.
The second layer in the walls is the submucosa that supports the mucous membrane. It is composed of connective tissue with elastic fibers.
The next layer is the muscularis, which is composed of smooth muscle. The smooth muscle fibers are interwoven in all directions and collectively these are called the detrusor muscle. Contraction of this muscle expels urine from the bladder. On the superior surface, the outer layer of the bladder wall is parietal peritoneum. In all other regions, the outer layer is fibrous connective tissue.
There is a triangular area, called the trigone, formed by three openings in the floor of the urinary bladder. Two of the openings are from the ureters and form the base of the trigone. Small flaps of mucosa cover these openings and act as valves that allow urine to enter the bladder but prevent it from backing up from the bladder into the ureters. The third opening, at the apex of the trigone, is the opening into the urethra. A band of the detrusor muscle encircles this opening to form the internal urethral sphincter.
Urethra
The final passageway for the flow of urine is the urethra, a thin-walled tube that conveys urine from the floor of the urinary bladder to the outside. The opening to the outside is the external urethral orifice. The mucosal lining of the urethra is transitional epithelium. The wall also contains smooth muscle fibers and is supported by connective tissue.
The internal urethral sphincter surrounds the beginning of the urethra, where it leaves the urinary bladder. This sphincter is smooth (involuntary) muscle. Another sphincter, the external urethral sphincter, is skeletal (voluntary) muscle and encircles the urethra where it goes through the pelvic floor. These two sphincters control the flow of urine through the urethra.
In females, the urethra is short, only 3 to 4 cm (about 1.5 inches) long. The external urethral orifice opens to the outside just anterior to the opening for the vagina.
In males, the urethra is much longer, about 20 cm (7 to 8 inches) in length, and transports both urine and semen. The first part, next to the urinary bladder, passes through the prostate gland and is called the prostatic urethra. The second part, a short region that penetrates the pelvic floor and enters the penis, is called the membranous urethra. The third part, the spongy urethra, is the longest region. This portion of the urethra extends the entire length of the penis, and the external urethral orifice opens to the outside at the tip of the penis.
Renal And Kidney
Renal And Kidney
Renal And Kidney
Renal And Kidney
Renal And Kidney
Renal And Kidney
Renal And Kidney
Renal And Kidney
Renal And Kidney
Renal And Kidney
Renal And Kidney